Insulin resistance is a condition where cells in the muscles, fat, and liver do not respond properly to insulin, a hormone that regulates blood glucose levels. Over time, insulin resistance can lead to prediabetes and Type 2 diabetes. Understanding the causes of insulin receptor desensitization is crucial for managing and preventing these conditions.
The Role of Insulin in Glucose Regulation
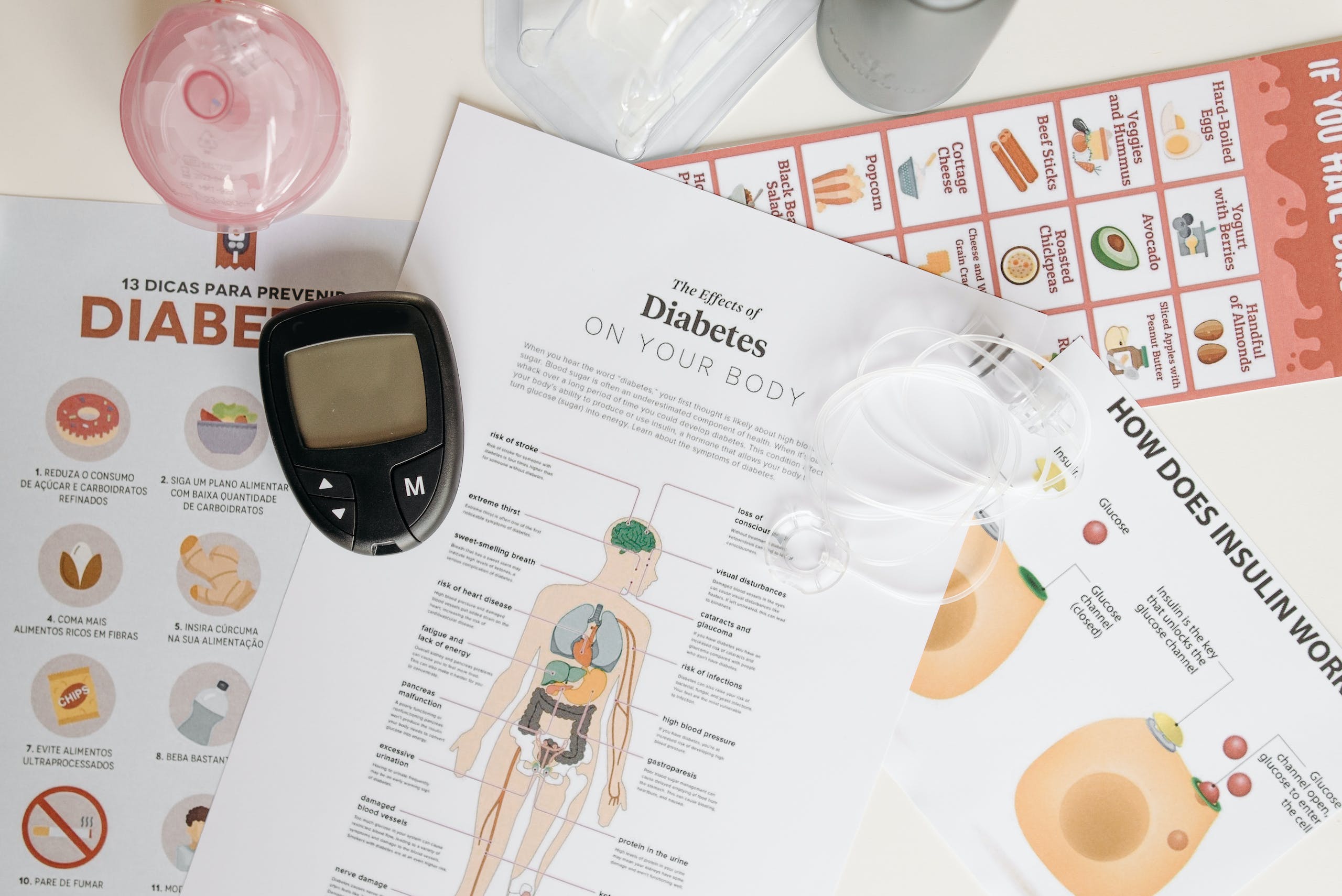
To understand insulin resistance, it’s important to grasp the normal function of insulin in the body. When you eat food, your body breaks down carbohydrates into glucose, which enters the bloodstream. In response, the pancreas releases insulin, which helps transport glucose into cells for energy or storage.
Under normal circumstances:
- Food is broken down into glucose.
- Glucose enters the bloodstream, triggering insulin release.
- Insulin enables cells to take up glucose for energy or storage.
- As glucose levels decrease, the pancreas stops producing insulin.
However, in cases of insulin resistance, cells do not respond effectively to insulin, leading to elevated blood glucose levels.
Causes of Insulin Resistance
Insulin resistance can be caused by various factors, including:
1. Excess Body Fat
One of the primary contributors to insulin resistance is excess body fat, especially around the abdomen. Adipose tissue, or fat cells, produce substances that can interfere with insulin signaling, leading to reduced sensitivity.
2. Lack of Physical Activity
A sedentary lifestyle can also contribute to insulin resistance. Regular physical activity helps improve insulin sensitivity, allowing cells to more efficiently take up glucose from the bloodstream.
3. Genetic Factors
Certain genetic factors can predispose individuals to insulin resistance. These genetic variations can affect insulin signaling pathways or the production of insulin receptors, leading to reduced insulin sensitivity.
4. Hormonal Imbalances
Hormonal imbalances, such as polycystic ovary syndrome (PCOS) or Cushing’s syndrome, can contribute to insulin resistance. These conditions affect hormone levels in the body, disrupting normal insulin function.
5. Chronic Inflammation
Chronic inflammation in the body can impair insulin signaling and contribute to insulin resistance. Inflammatory substances released by immune cells can interfere with insulin receptor activity.
6. Medications and Medical Conditions
Certain medications, such as corticosteroids, can induce temporary insulin resistance. Additionally, medical conditions like gestational diabetes during pregnancy can cause insulin resistance, which usually resolves after delivery.
It’s important to note that insulin resistance can affect anyone, regardless of whether they have diabetes. However, individuals with prediabetes and Type 2 diabetes often have some level of insulin resistance.
The Link Between Insulin Resistance and Diabetes
Insulin resistance is closely linked to the development of prediabetes and Type 2 diabetes. Prediabetes occurs when blood glucose levels are higher than normal but not yet in the diabetes range. If left untreated, prediabetes can progress to Type 2 diabetes.
Type 2 diabetes occurs when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. This results in persistently high blood glucose levels.
On the other hand, Type 1 diabetes is an autoimmune condition where the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. While not caused by insulin resistance, individuals with Type 1 diabetes can still experience insulin resistance to some extent.
The Impact of Insulin Resistance on the Body
Insulin resistance can have various effects on the body, including:
1. Hyperinsulinemia
When cells become resistant to insulin, the pancreas compensates by producing more insulin. This can lead to a condition called hyperinsulinemia, characterized by elevated insulin levels in the blood. Prolonged hyperinsulinemia can contribute to weight gain and worsen insulin resistance.
2. Increased Risk of Type 2 Diabetes
If insulin resistance persists and the pancreas cannot produce enough insulin to overcome it, blood glucose levels continue to rise, leading to the development of Type 2 diabetes. Individuals with insulin resistance are at a higher risk of developing this chronic condition.
3. Metabolic Syndrome
Insulin resistance is a key feature of metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and Type 2 diabetes. Metabolic syndrome is characterized by elevated blood glucose levels, high blood pressure, low levels of HDL cholesterol, and increased triglyceride levels.
4. Cardiovascular Disease
Insulin resistance and metabolic syndrome are both associated with an increased risk of cardiovascular disease. The combination of elevated blood glucose levels, high blood pressure, and abnormal lipid profiles can damage blood vessels and increase the likelihood of heart disease.
Diagnosis of Insulin Resistance and Diabetes
Healthcare providers use various tests to diagnose insulin resistance and diabetes. One commonly used test is the glycated hemoglobin (A1c) test, which measures average blood sugar levels over the past three months.
The diagnostic criteria are as follows:
- A1c level below 5.7%: Normal
- A1c level between 5.7% and 6.4%: Prediabetes
- A1c level of 6.5% or higher on two separate tests: Type 2 diabetes
It’s important to note that individuals with Type 1 diabetes typically have very high A1c levels and blood glucose levels upon diagnosis due to the lack of insulin production.
Prevention and Management of Insulin Resistance
While certain factors contributing to insulin resistance, such as genetics, cannot be changed, there are steps individuals can take to prevent or manage insulin resistance and its associated conditions:
1. Maintain a Healthy Weight
Losing excess body fat, particularly around the abdomen, can improve insulin sensitivity. Engaging in regular physical activity and adopting a balanced, nutritious diet are key components of weight management.
2. Stay Active
Regular exercise helps improve insulin sensitivity and can aid in weight management. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with strength training exercises.
3. Follow a Balanced Diet
Focus on consuming nutrient-dense foods, including whole grains, lean proteins, fruits, and vegetables. Limit the intake of sugary beverages, processed foods, and foods high in saturated and trans fats.
4. Monitor Blood Glucose Levels
Individuals at risk of insulin resistance or diabetes should monitor their blood glucose levels regularly. This can help detect any abnormalities early and allow for prompt intervention.
5. Manage Stress Levels
Chronic stress can contribute to insulin resistance. Implement stress management techniques such as meditation, deep breathing exercises, or engaging in hobbies to reduce stress levels.
6. Consult with Healthcare Professionals
If at risk or experiencing symptoms of insulin resistance or diabetes, consult with healthcare professionals. They can provide personalized guidance, recommend appropriate lifestyle changes, and prescribe any necessary medications.
The Bottom Line
Insulin resistance is a condition where cells do not respond properly to insulin, leading to elevated blood glucose levels. It is a precursor to prediabetes and Type 2 diabetes, and it is associated with various health risks, including cardiovascular disease and metabolic syndrome. Understanding the causes of insulin resistance and implementing preventive measures can help individuals maintain optimal health and reduce the risk of developing chronic conditions. By maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet, individuals can improve insulin sensitivity and overall well-being. Regular monitoring and consultation with healthcare professionals are essential for early detection and management of insulin resistance.